The Silent Epidemic Robbing America of Restful Nights
Roughly one in ten adults across the United States now admits to battling chronic insomnia—yet that sobering figure barely captures the broader crisis. Surveys indicate that tens of millions more routinely wake up feeling far from refreshed. Behind those restless nights, scientists are uncovering alarmingly tight links to long-term ailments, most notably cardiovascular disease. In a recent dialogue organized by The Conversation and SciLine, Dr. Julio Fernandez-Mendoza—professor of psychiatry, behavioral health, neuroscience, and public health sciences at Penn State College of Medicine—offers clarity on why shut-eye matters, how adolescents are uniquely vulnerable, and practical steps to reclaim restorative sleep without turning to pharmaceuticals.
Why the Body Demands High-Quality Sleep
- Cardiovascular vigilance: Inadequate rest triggers inflammatory pathways that quietly injure vessel walls, setting the stage for heart disease years before symptoms appear.
- Cognitive housekeeping: Deep, slow-wave sleep scrubs metabolic waste from the brain—miss these cycles and next-day focus drops measurably.
- Metabolic reset: Sleep curbs ghrelin (the hunger hormone) while elevating leptin (the satiety signal), helping the body balance energy use overnight.
Teenagers Are Especially Sleep-Debt Deficient
The biological clock during adolescence shifts later, making early school start times a collision course with natural rhythms. Research confirms teens need 8.5–9.5 hours nightly—well above the adult norm—because their brains are undergoing massive pruning and myelination that sculpt lifelong neural architecture. Chronic curfew violations on weekdays, followed by weekend catch-up sessions, backfire by creating a perpetual jet-lag sensation known as social jet lag.
Practical Strategies for Medication-Free Rest
- Anchor wake time: Get up at the same moment seven days a week—even after a rough night—to stabilize circadian oscillations.
- Create a wind-down runway: Thirty to sixty minutes of dim lights and screen-free activity (light stretching, reading fiction) gives the brain permission to power down.
- Cool the bedroom: Set temperature roughly three degrees below daytime comfort; core body temperature must drop to initiate melatonin release.
- Watch the last call—caffeine: Finish any coffee, tea, or energy drinks by 2 p.m. at the latest; caffeine’s half-life lingers well into the evening.
- Banish midnight clocks: Cover glowing displays; clock-watching spikes cortisol and resets the mental racecar to “go” every time you check.
Key Takeaway
Sleep is not an optional luxury; it is a biological imperative intertwined with heart health, metabolic balance, and cognitive resilience. Adolescents require an even larger nightly allowance, and adults of every age can outsmart insomnia by syncing lifestyle habits to the body’s built-in rhythms—no prescription required.
How much sleep is enough for adults and for adolescents?
Goldilocks Sleep: How Much Is “Just Right?”
Most adults thrive on seven to eight hours of nightly rest, a sweet spot linked to lower rates of heart disease, sharper cognitive performance, and longer life expectancy. Yet this guideline is not one-size-fits-all; it grows more flexible with age, says sleep scholar Julio Fernandez-Mendoza.
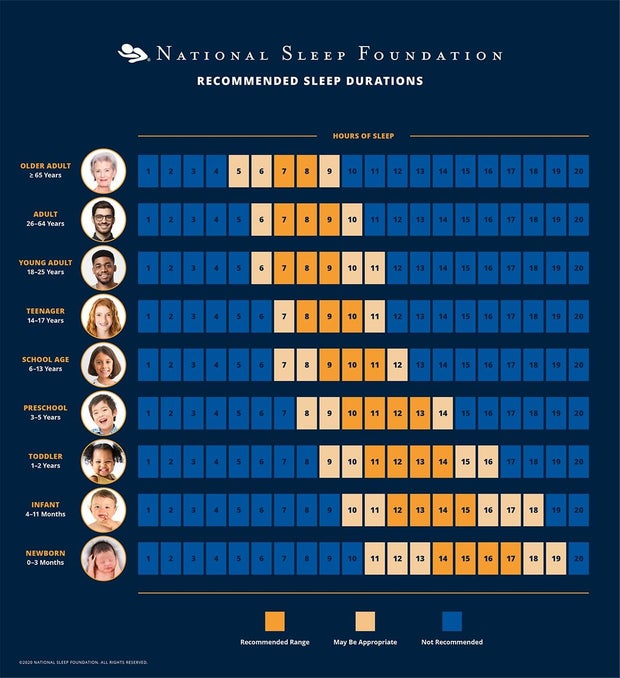
Age-Specific Sleep Targets
- Young children – often require well over nine hours, the precise amount determined by growth spurts and daily activity levels.
- Adolescents and young adults – should aim for at least nine hours to support learning, memory, and mood regulation.
- Middle-aged adults – the classic seven–to–eight-hour range remains optimal.
- Older adults (65+) – healthy seniors may flourish on six to seven hours, with no need for alarm when mornings start a bit earlier than in younger years.
Takeaway
If you are in good general health and logging roughly the hours listed above, there is no reason to fret over minor nightly variations. Match your pillow time to your life stage, and the benefits—both mental and physical—should follow naturally.
How can insufficient sleep harm our health?
Insomnia Poses an Early Warning for the Heart, Not Just a Nighttime Annoyance
New findings from Fernandez-Mendoza’s research team highlight a striking reality: trouble falling or staying asleep is not a harmless irritation—it quietly nudges blood pressure upward and sets the stage for cardiovascular disease long before a formal diagnosis appears.
Key Revelations from the Study
- Elevated Blood Pressure. Adolescents and adults who reported persistent insomnia were significantly more likely to cross into hypertensive territory.
- Inflammatory Cascade. Laboratory measures revealed heightened inflammatory markers and stress hormones in those with shortened, fragmented sleep.
- Sequence Matters. Sleep problems often surfaced ahead of any clinical signs of heart disease, indicating a critical early-intervention window.
Why Insomnia Triggers Heart Strain
Shortchanged sleep appears to rev up the sympathetic nervous system, pushing adrenaline and cortisol levels higher overnight. Over time, that nightly surge keeps blood vessels tense and inflammation simmering. The result: rising blood pressure and an immune system stuck in low-grade attack mode, both of which chip away at cardiovascular resilience.
What This Means for Clinicians & the Public
Screening for insomnia deserves a permanent seat beside blood-pressure and weight checks in routine visits. Offering cognitive-behavioural techniques for sleep, rather than waiting for cardiac symptoms to erupt, could tilt the risk curve away from future heart disease for millions of teens and adults.
The Surprising Truth About Sleep Needs Later in Life
Less, not more, shut-eye becomes standard once we blow out a few extra birthday candles. Health authorities have quietly revised the nightly sleep target for every decade after our early twenties, trimming off roughly 30–60 minutes per milestone. By the time we reach retirement, most healthy adults are judged to need a solid seven hours, sometimes even six and a half, rather than the eight that is advertised for everyone.
How the Numbers Shrink Over the Decades
- Young adults (18–25): 7–9 hours widely encouraged for peak cognitive and muscular recovery.
- Middle-age group (26–64): Guidance narrows toward 7–8 hours, with flexibility for an extra nap on demanding days.
- Older adults (65 and up): Seven hours can be sufficient, and many feel genuinely restored at 6.5–7.5 hours.
Why the Drop Makes Biological Sense
Neurologists point to slower brain-wave activity in deep sleep phases and a natural shift in circadian rhythm. Together these changes allow more restorative power per minute, letting seniors spend a shorter stretch in bed while still earning the full dividend of physical repair and memory consolidation.
Myth-Busting the “8-Hour Rule”
Blanket recommendations overlook age, fitness, and even chronic conditions. A 70-year-old marathon runner may thrive on six and a half hours; a sedentary 40-year-old might actually need eight and a half. The real cue is day-time alertness, not a stopwatch under the pillow.
Take-Home Checklist
- Note how you feel before caffeine at lunchtime. Grogginess = deficit.
- Track total sleep (not just bedtime) for two weeks—phones and wearables do the math.
- Adjust in 15-minute increments. Aim for the minimum block that leaves you clear-headed, mood-stable, and productive.
What about people who have more serious sleep problems?
Sleep Like a Pro: The Six-Pillar Blueprint for Defeating Insomnia
While trimming caffeine and keeping bedtime snacks light are great first steps, lasting relief from stubborn sleepless nights often demands a deeper reset. Fernandez-Mendoza distills decades of clinical research into six non-negotiable behavioral pillars that outperform basic sleep tips. Commit to them for a few weeks, then tailor them to fit your lifestyle.
Pillar 1 – Lock-and-Load Wake Time
Rise at exactly the same hour every single morning—weekends included—regardless of how little sleep the night granted. Your circadian anchor cannot adjust to mixed signals.
Pillar 2 – The Bedroom’s “Jobs Description”
- Sleep
- Sex
- Nothing else—no scrolling, spreadsheets, or snack attacks.
Pillar 3 – The 20-Minute Rule
Still staring at the ceiling after 20 minutes? Move to another room and engage a soothing activity—light fiction, easy stretching, soft music. Return only when true sleepiness returns.
Pillar 4 – No Sleep Rebound Tactics
Forgo naps, extra espresso, or that “quick doze” on the sofa after a rough night. They scatter the body’s pressure to sleep later, extending the cycle of insomnia.
Pillar 5 – Bedtime by Biology, Not Clock
The mattress is reserved solely for those moments when eyelids feel heavy and you’re genuinely ready to drift off. Forced early lights-out trains the body to fight rather than surrender.
Pillar 6 – Graduated Sleep Expansion
- Start at 5 hours minimum nightly—even if it means a later bedtime.
- Add 15 minutes per week until mornings feel refreshing.
- Hold at that new duration for at least three consecutive well-rested days before pushing further.
When to Seek Expert Guidance
Give this regimen four to six disciplined weeks. Persisting issues warrant professional evaluation; behavioral or cognitive interventions can provide the targeted fine-tuning these rules cannot.
Do you have advice specifically for adolescents?
Why Your Teen Feels like a Night Owl: A Behind-the-Scenes Look at Adolescent Sleep
Fernandez-Mendoza pulls back the curtain on a hidden revolution unfolding inside every teenager. Adolescence isn’t merely a parade of growth spurts, mood swings, and louder music choices; it’s brain renovation on a grand scale. During this overhaul, the body quietly resets a master clock that decides when we feel sleepy and when we feel sharp. That tiny reset can turn even the most enthusiastic early-morning student into the last one standing at 2 a.m.
The New Rhythm: Biology Beats Intention
- At puberty, the suprachiasmatic nucleus—your teen’s internal metronome—slides forward, making 10 p.m. feel like early evening.
- The urge to text, game, or chat may amplify the late-night vibe, but it is the shifted circadian phase that plants the fundamental seed.
- Early bell schedules clash with this biology, slicing off precious hours of restorative slow-wave sleep and blunting memory, mood, and grades.
School Bells vs. Body Clocks
A growing stack of studies
reveals districts that push first period past 8:30 a.m. see higher attendance, better test scores, and fewer car-pool yawns. In short, aligning classrooms with circadian science is less luxury, more necessity.
Coach at Home: How Parents Can Hack the Clock—Gently
- Curfew the devices. Pick a “screens-off” hour—say 9:30 p.m.—and trade the phone for a shared sitcom episode or a dog-eared fantasy novel.
- Creep the wake-up. Slide alarm clocks earlier in 15–30-minute increments, weekends included, until the goaltime emerges naturally. Abrupt 5 a.m. drills backfire; evolution can’t sprint.
- Watch red flags. After six consistent weeks, if your child still can’t drift off or struggles to wake, loop in a sleep clinician. There may be insomnia, delayed-phase disorder, or another treatable hiccup at play.
Bottom Line
Your teenager’s late-night energy isn’t rebellion—it’s physiology wearing sneakers. A classroom that starts later, paired with tiny, thoughtful tweaks at home, can turn sleepless nights into bright mornings without a single battle.
What kind of treatments can a sleep clinician provide?
A Wake-Up Call From a Sleep Specialist: Your Symptoms Deserve Action
Red Flags You Should Never Ignore
- Troubled sleep that takes forever to start or stay continuous.
- Overwhelming daytime fatigue, even after what felt like a full night.
- Nocturnal sounds and motions such as loud snoring or chronic teeth-grinding.
According to sleep researcher Fernandez-Mendoza, any of these indicators justify a timely conversation with a qualified professional.
What a Sleep Visit Really Looks Like
Contrary to widespread belief, a referral to a sleep provider does not obligate you to pricey prescriptions. Instead, modern clinics emphasize:
- Cognitive Behavioral Therapy for Insomnia (CBT-I) – the gold-standard, non-pharmacological program that retrains your mind and body for restorative sleep.
- Light Therapy – timed exposure to a medical-grade lamp to reset circadian rhythms, tailored to each patient’s unique schedule.
- Numerous other lifestyle or behavioral tweaks that require little to no medication at all.
About the Expert Source
This guidance is excerpted from an in-depth conversation featured by SciLine, a no-cost resource housed within the American Association for the Advancement of Science. SciLine was created to help journalists weave trustworthy scientific evidence and expert voices into every story they report.

From Labs to Lockdowns: How One Tiny Variant Upended the World
When a Molecule Becomes a Headline
Until the last days of 2019, the word “coronavirus” lived only in scientific journals and hospital bulletin boards. Then a single mutation-prone pathogen turned airport terminals into ghost towns, school corridors into silence. Virologists who once spoke in footnotes suddenly stood beside presidents, their charts dictating border closures that separated families overnight.
The Science Whispers First
- On Christmas Eve, a Wuhan clinic logs an unusual cluster of pneumonia cases.
- Three days later, gene sequencers spit out R-a-t-g-13—the closest known cousin in bats.
- By New Year’s, the sequence is in a global repository, an act of openness that becomes a lifeline for vaccine designers racing against time.
The Dominoes Fall Faster Than Data
Stockholm to São Paulo, governments face the same impossible equation: How do you slow a microbe when each flight is a booster shot for its spread? Politicians trade nightly calls with epidemiologists, then translate exponential curves into curfews, mask mandates, and trillion-dollar rescue packages.
Inside the War Rooms
Britains’s SAGE committee meets over Zoom, faces framed on laptops like Hollywood squares, debating the R number the way generals once debated beachheads.
In Pretoria, modellers run scenarios showing an entire country’s oxygen inventory exhausted within 11 days if nothing changes.
A Chronicle Written by All of Us
The story belongs to more than labs and legislatures. It is woven in sourdough starters at 2 a.m.; in drive-by birthdays; in the shaky voice of a nurse turning an iPad so a grandmother can meet her newborn granddaughter through plastic. These fragments, mundane and extraordinary, form the human ledger of a pandemic that no spreadsheet could trace.
What began as faint data points on a virology screen has become a history still being told—through antibody curves and anniversary candles, through each breath we remember we’re lucky to take.




