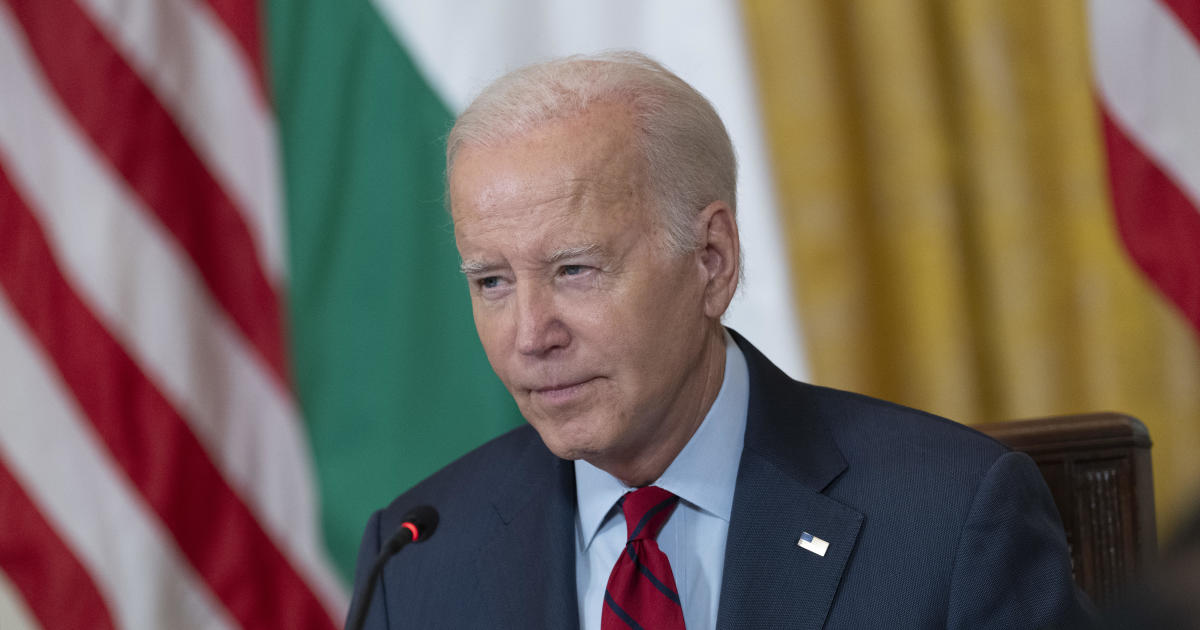
President Biden Turns to CPAP Therapy for Restful Nights
The White House acknowledged on Wednesday that President Joe Biden has begun using a continuous positive airway pressure (CPAP) device—an apparatus designed to keep airways open during sleep—to counter longstanding sleep apnea.
Eight Decades of Life, Decades of Breathing Trouble
- Biden first told his physicians about sleep-disordered breathing back in 2008.
- Medical files list the condition under “resolved” episodes, yet clinicians still monitor lingering patterns.
- With roughly 30 million other Americans facing the same diagnosis, the President joins a sizable cohort of nighttime CPAP users.
Inside the Bedroom: How the Machine Works Overnight
The apparatus delivers steady pressurized air through a lightweight mask, preventing throat tissues from collapsing. A senior White House aide noted simply, “He switched it on last night, consistent with anyone who shares the same medical background.”
Fast Facts on Sleep Apnea
- Sleepers stop breathing momentarily, sometimes dozens of times an hour.
- Severe cases raise risks for hypertension, stroke, and heart disease.
- CPAP therapy remains the frontline treatment, offering improved rest and daytime alertness within weeks.
Why the Revelation Matters Now
The disclosure comes amid heightened scrutiny of Biden’s overall vigor ahead of an anticipated re-election campaign. Supporters argue that proactive treatment demonstrates attentiveness to health, while critics seek fuller medical briefings. For millions of voters wrestling with similar nighttime breathing challenges, the President’s adoption of CPAP may resonate more as a shared daily routine than a campaign footnote.
What is sleep apnea?
Sleep Apnea Uncovered: The Silent Night-Time Threat Affecting One in Seven People
While most of us think of sleep as one long, uninterrupted rest, hundreds of millions slip into a nightly struggle in which breathing stops, sometimes for a dozen seconds at a time, then restarts with a gasp. This phenomenon—sleep apnea—is not just a noisy nuisance; experts now call it a global health emergency lurking in the dark.
Who Faces the Highest Danger?
- Sex: Men remain far more likely to develop the disorder.
- Age: Risk rises sharply after 40 and escalates throughout later life.
- Weight: Excess body fat around the neck and chest narrows airway space.
- Lifestyle Triggers: Evening cocktails, cigarettes, or opioid painkillers all relax throat muscles or dampen the brain’s breathing reflex.
The Two Masked Offenders
Obstructive Sleep Apnea (OSA)
Picture a balloon collapsing as someone repeatedly pinches the opening—this is how soft throat tissue obstructs the airway every few minutes, cutting off oxygen until the sleeper jerks awake to reopen the passage. The National Institutes of Health label OSA the most widespread type and the one snoring spouses often hear first.
Central Sleep Apnea (CSA)
In CSA, there’s no physical blockage; instead, the brain’s “breathe now” signal stalls, leaving the lungs perfectly clear yet momentarily idle. Think of it as a missed drumbeat in the body’s internal marching band.
The Hidden Ocean of the Undiagnosed
Dr. Carlos M. Nunez, former intensive-care physician and present Chief Medical Officer at ResMed, offers a staggering statistic: “Roughly one billion people worldwide have sleep apnea, yet more than eighty percent remain undiagnosed and untreated.” That makes the disorder more prevalent than diabetes and asthma combined, operating mostly in silence.
Why Your Silence at 3 A.M. Could Shout Trouble by 50
The nightly oxygen dips are more than fatigue generators. They are micro-assaults that gradually raise the body’s inflammatory burden, setting the stage for serious downstream illnesses.
- Heart and Blood Vessels: Persistent low oxygen stresses arteries, driving hypertension, atrial fibrillation, heart attacks, and strokes.
- Brain Aging: Fragmented sleep starves neurons of restorative deep stages, accelerating tau tangles and beta-amyloid plaques—a recognized pathway toward Alzheimer’s disease and other forms of dementia.
- Metabolic Mayhem: Poor sleep sabotages insulin sensitivity, increasing the odds of type 2 diabetes.
Sounding the Alarm Early
If you snore thunderously, wake feeling unrefreshed, or a bed partner reports pauses in your breathing, act now:
- Ask a primary-care physician or a certified sleep specialist for a screening questionnaire.
- Consider an overnight sleep study, now available in many homes via portable monitors.
- Start positive lifestyle tweaks—losing 10% of body weight can reduce episodes by half; skipping the nightcap removes another chokehold on the airway.
Early discovery today buys peaceful nights—and longer, clearer tomorrows. Every breath, even the ones after midnight, counts.
Symptoms of sleep apnea
Could Your Snore Be a Red Flag? The Quiet Clues of Hidden Sleep Trouble
Tired by 10 a.m., jolted awake at 2 a.m., greeted each dawn by a Sahara-dry mouth—if this sounds familiar, the National Institutes of Health warn these are classic fingerprints of obstructive sleep apnea (OSA).
Five Whispers Your Body Sends at Night
- Unshakable daytime sleepiness no matter how long the night
- Breathing pauses noticed by a bed-partner between long, loud cycles
- Echoing, room-shaking snores
- Gasping or choking sounds that yank you back to the surface of sleep
- Morning headaches and a tongue that feels stapled to the roof of your mouth
Louder Than Words: When Snoring Ceases to Be “Normal”
Every sleeper on the planet can snore, yet only a fraction are in danger. Dr. Nunez separates the background noise from the siren call:
“It’s not the gentle rumble that melts into silence. It’s snoring so forceful the walls seem to vibrate, or it’s punctuated by sudden, eerie silence—like someone swallowed their own airway. The choking that follows is the giveaway.”
What is “Sleep Banking” and Can It Help You Feel Brighter?
Sleep banking flips the standard advice on its head. Instead of only trying to undo the damage after the fact, you pre-load extra hours on nights when you are still in control.
How to Build Your Own Sleep Bank
- Add 30 – 60 extra minutes for four to five days before an expected period of sleep loss
- Keep consistent bedtime and wake-up times to anchor your circadian rhythm
- Dial back caffeine after 2 p.m. so the bonus sleep is truly restorative
- Reserve the last 20 minutes before lights-out for quiet, low-stimulus activities
Newer studies show the banked sleep can shave drowsiness, boost reaction time, and even lower the intensity of apnea events in borderline cases—though it is no replacement for a CPAP if you already have moderate to severe OSA.
Bottom line: Loud, choking snores plus morning fog should prompt a professional evaluation. Once treated, a little strategic sleep banking could give you a buffer against the occasional late-night Netflix binge or an early flight.
Sleep apnea treatment
What’s Inside Your Nighttime Tabletop Turbine?
Millions of people slip on a mask each evening not to go scuba-diving in their living rooms, but to meet a tiny box of wind at their bedside. That box—technically called continuous positive airway pressure equipment—has become the Swiss Army tool for fighting obstructed breathing during sleep.
How the Gadget Turns Breath into Balloon-Pressure
- A motor hums like a miniature vacuum in reverse. It spins up, drawing room air through a replaceable filter.
- Humidification chamber steams the flow. Water heats to moisten the breeze so throats, noses, and sinuses do not feel like parchment by 4 a.m.
- Tubes snake out like flexible garden hoses. They transport the now-warm, filtered air across pillows and sheets to the sleeper.
- The mask seals—gently, not vise-tight. Nasal pillows, full-face domes, or simple nasal cones channel the breeze precisely where needed.
- Air puffs act like splints. Instead of metal or plastic, the air column props open soft tissues at the back of the throat, keeping the airway patent all night.
Real-Life Scenes You Might Recognize
Before the Machine Joins the Bedside
Snoring rattles the walls, a partner retreats to the couch, and daytime brain-fog feels like wading through peanut butter.
First Week with the Wind
- Mask straps mark cheeks like gentle caterpillars.
- Humidifier water vanishes faster than a midnight snack.
- Morning one: the brain is still foggy, but energy rises marginally enough to notice the difference.
Months Later
Coffee may stay in the cupboard until after 9 a.m. The partner reclaims their side of the bed. And the once-deafening snore has faded to a polite exhale.

Modern CPAP Therapy: Quiet, Smart, and Far More Comfortable Than You Remember
Sleep apnea remains one of the most under-diagnosed disorders in the United States, yet the tools used to treat it have quietly transformed into sleek, data-rich devices that look nothing like the bulky, hissing machines of decades past.
The Myth of the “Clunky” CPAP Dies Hard
Few medical devices carry as many outdated mental images as the CPAP.
“It’s understandable,” notes respiratory therapist Luis Nunez. “When people hear CPAP, they still picture a refrigerator-sized box blasting like a leaf blower.” He calls that portrayal purely historical. Today’s machines are whisper-quiet units about the size of a paperback novel, capable of logging every breath, heartbeat, and micro-arousal through the night.
Beneath the Mask: How Technology Rebuilt Trust
What Has Actually Changed
- Sound: Current models operate below 26 dB—quieter than most libraries.
- Fit: Mask options range from feather-light nasal pillows to ultra-flexible full-face gaskets.
- Data: Built-in cellular or Bluetooth chips stream metrics—hours of use, leak rates, AHI trends—straight to clinicians and patients.
- Adherence: Early studies show a 25–30 % increase in nightly use when patients can watch their progress in real time on a smartphone.
The psychological boost is equally striking, says Nunez. “Give someone a device that talks back with encouraging stats, rather than vague doctor visits weeks away, and long-term use climbs dramatically.”
Beyond the Machine: Lifestyle, Surgery, Sleep Labs
First-Line Lifestyle Tweaks
- Dropping 10 % of body weight can cut apnea events by up to 50 %.
- Cutting alcohol within four hours of bedtime reduces upper-airway collapse.
- A firm quit-smoking plan lowers inflammation and nighttime congestion.
When Extra Help Is Needed
Sleep study labs (either in-center or home-based) remain the gold standard for diagnosis. If nightly airflow remains insufficient after weeks of diligent CPAP use and lifestyle changes, physicians may recommend minimally invasive surgeries—such as uvulopalatopharyngoplasty or hypoglossal nerve stimulation—to reopen the airway at its root.
A Call to the Undiagnosed
Loud snoring, daytime fatigue, and morning headaches are not inevitable aspects of aging. A single overnight assessment paired with one of the new-generation CPAP systems can convert restless nights into 8 hours of steady, oxygen-rich rest. As Nunez summarizes, “Today’s therapy feels less like medical machinery and more like wearable technology—finally worthy of actually wanting to use.”